75 YEAR OLD MAN WITH FEVER AND THROMBOCYTOPENIA
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
Here is a case i have seen:
A 75 year old male farmer by occupation was brought to the opd by his wife and son-in-law with
chief complaints of
Polyuria since 5 years
Dyspnea on exertion since 2 years
Abdominal distension since 2 years
Fever associated with body pains since 3 days
He used to work as a farmer 3 years back in a small village near Nalgonda.
History of present illness:
patient was apparently alright 5 years back ,then he says that he has to get to use the washroom multiple number of times since the past 5 years, he then visited the hospital to get a diabetic work up done. He was diagnosed to be hypertensive and was started on medication.
Over the past 2 years he has been finding it difficult to work as he started to get dyspneic after walking for short distances and his abdomen was distended. He visited local hospitals twice and he was told he had nothing to worry about. Over the last 2 months his dyspnea and abdominal distension have comparatively aggravated.
Since the past 3 days he has been having fever associated with chills and Boyd pains, which was continuous. He visited a local hospital where in, he received certain medications including Inj Monocef and paracetamol. He was told that he had really low platelet count and would be better if he visited another hospital.
personal history:
He has been an alcoholic and a beedi smoker over 30 years. He drinks around 90-180 ml of whiskey every day especially over the last 3 years he hasn’t been working. His last intake was 10 days back.
Past history:
He is a K/C/O hypertension since 3 years and is on Tab. Atenolol 50mg PO BD. He also gives a H/O constipation for the past few weeks.
Not a K/C/O DM, epilepsy, CAD, asthma, TB.
General examination:
Patient is conscious, cooperative.
Temperature: 99.4 degrees F
Pulse rate: 62 beats per minute
Respiratory rate: 18 cycles per minute
BP : 110/70 mm of hg
Spo2: 98% at room air.
systemic examination:
CVS: S1, S2 +
RS: Dyspnoea Grade III (on exertion) , BAE + ,
Fine Crepts + B/L IAA , ISA
PA : soft, distended,non tender , bowel sounds +
CNS: intact
INVESTIGATIONS:
dengue NS1 antigen .positive
CBP:
LFT:
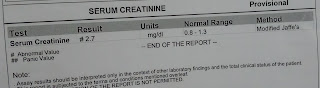
RFT:
2 NS 75ml/hr
2)inj pantap 40 mg iv od before breakfast
3)inj zofer 4 mg i.v sos
4) tab dolo 650 mg po bd
5)inj optineuron 1 amp in 100 ml NS/i v/od
C/O SOB GRADE 1-2
PASSED STOOLS
PLUS IV FLUIDS 2 NS SND 2 DNS @100ML/HR
2 .INJ.OPTINEURON 1 AMP IN 100 ML NS IV OD
3.TAB.DOLO 650 MG PO BD
4.INJ.PAN 40 MG IV OD
5.INJ.ZOFER 4MG IV SOS
C/O SOB GRADE 1-2
PASSED STOOLS
1.PLENTY OF ORAL FLUIDS 3L PER DAY
PLUS IV FLUIDS 2 NS SND 2 DNS @100ML/HR
2 .INJ.OPTINEURON 1 AMP IN 100 ML NS IV OD
3.TAB.DOLO 650 MG PO BD
4.INJ.PAN 40 MG IV OD
5.INJ.ZOFER 4MG IV SOS
C/O SOB GRADE 1-2
2 EPISODES OF LOOSE STOOLS YESTERDAY
1.PLENTY OF ORAL FLUIDS 3L PER DAY
PLUS IV FLUIDS 2 NS SND 2 DNS @100ML/HR
2 .INJ.OPTINEURON 1 AMP IN 100 ML NS IV OD
3.TAB.DOLO 650 MG PO BD
4.INJ.PAN 40 MG IV OD
5.INJ.ZOFER 4MG IV SOS
6.TAB.AMLONG 5 MG PO OD
PLUS IV FLUIDS 2 NS SND 2 DNS @100ML/HR
2 .INJ.OPTINEURON 1 AMP IN 100 ML NS IV OD
3.TAB.DOLO 650 MG PO BD
4.INJ.PAN 40 MG IV OD
5.INJ.ZOFER 4MG IV SOS
6.TAB.AMLONG 5 MG PO OD













Comments
Post a Comment